High Risk Groups
High-Risk groups for Adrenal Crisis include:
From my own clinical experience, the most vulnerable patients are those with primary adrenal deficiency, especially when linked to congenital hyperplasia, Addisons disease, or adrenal hypoplasia. I’ve also seen risks in secondary pituitary ACTH deficient conditions, such as Hypopituitarism, whether congenital or idiopathic, often associated with rare structural issues like Septo-optic dysplasia, midline CNS abnormalities, or even tumours involving the suprasellar region. Another group I pay close attention to are those who have had recent treatment with high dose synthetic steroids for prolonged periods, particularly if they suddenly discontinued their therapy or were on long-term dexamethasone, since this abrupt change can trigger crisis quickly.
Background
The classic triad of a primary adrenal crisis often shows up in both lab findings and physical symptoms. From my own observation, it’s rarely straightforward—patients present with a cluster of subtle signs that can quickly escalate.
Key Laboratory Clues
| Marker | Abnormality in Adrenal Crisis |
| Serum Na | Low (hyponatremia) |
| Serum K | High (hyperkalemia) |
| Glucose | Low (hypoglycemia) |
Common Symptoms and Signs
- Severe dehydration leading to shock
- GI complaints: vomiting, diarrhoea, abdominal pain, sometimes constipation
- Fainting spells (syncope) with postural drop in BP
- Systemic features: fever, tachycardia, hypotension, metabolic acidosis
- Neurological: lethargy, profound weakness
In one case I recall, the subtle onset of weakness and mild abdominal pain was dismissed until the sudden collapse from hypotension revealed the underlying adrenal failure.

Investigations
When evaluating for adrenal crisis, both blood tests and clinical tests are vital. A structured approach not only helps confirm the diagnosis but also highlights the severity of cortisol deficiency.
Blood Tests
| Test | Purpose | Abnormal Findings |
| Electrolytes (Na, K, Calcium) | Detect imbalance | Low Na, High K, Low/Normal Calcium |
| Glucose | Check for metabolic derangement | Low (hypoglycemia) |
| Renal function | Assess kidney stress | Elevated urea/creatinine |
| FBC | Look for infection or stress response | Leukocytosis or anemia |
| CRP | Identify inflammation/infection | Elevated in stress or infection |
| Cap gas & lactate | Detect metabolic state | Acidosis, raised lactate |
Clinical Tests
- Monitor vital signs: BP, Pulse, Temperature
- Look for Postural Hypotension as an early warning signal of severe cortisol deficiency
- Maintain accurate fluid balance to guide resuscitation and avoid overload
In my experience, the signals often appear in the vitals before labs come back—an unexplained drop in BP or rising pulse can be the first clue that points to a crisis.
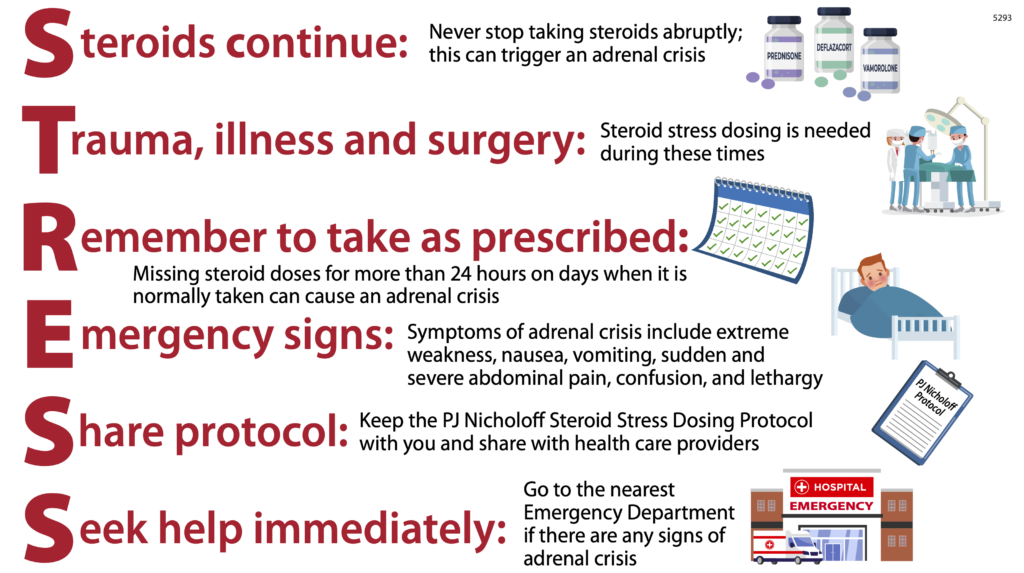
Principles of management
In normal subjects, cortisol levels naturally increase several-fold during physical stress, whether from major illness, anaesthesia, or surgery. But in children and adults with adrenal insufficiency, this stress response is absent, so the goal is to replace it with an appropriate response.
Steroid Choice & Route
| Steroid | Preferred Route | Notes |
| Hydrocortisone | IV / IM | Steroid of choice, rapid onset |
| Continuous infusion | IV | Ideal for maintaining steady levels |
| Intermittent boluses | 6-hourly / per day | Practical option when infusion not possible |
| Dexamethasone | IV | Exception: no mineralocorticoid effect, useful if diagnosis uncertain |
| Prednisone | PO | Can continue if patient can tolerate PO |
Dosing Strategy
- Stat bolus followed by total 24-hour period coverage
- Either continuous infusion or divided intermittent boluses
- High doses may be required in severe cases to ensure sufficient cortisol replacement
- Add fludrocortisone for mineralocorticoid effect, unless already covered by hydrocortisone
Practical Considerations
- Keep replacement short and simple—patients often recover within 48 hours
- Begin tapering in the appropriate setting rather than stopping abruptly
- Always search for the underlying cause such as occult infection (e.g., appendicitis, UTI) that may be masked by medication
- Use Table equivalent doses when switching between steroids for clarity and safety
From my own experience, starting with a stat dose and closely watching the fluid balance often makes the difference between stability and rapid deterioration. The tapering step is just as important—if you stop completely without covering the stress period, relapse can occur quickly.
Management details
A – Severely Unwell
In a crisis, a severely unwell patient—often unstable, vomiting, with diarrhoea, or too drowsy to tolerate oral hydrocortisone—requires urgent intervention. The initial bolus, IV fluids, and rapid steroid replacement form the backbone of management.
Immediate Steps
- Give Bolus IV fluids: 10–30 mL/kg 0.9% saline for resuscitation
- Switch to maintenance with 5% dextrose to prevent hypoglycemia
- Start steroids without delay:
- Hydrocortisone 75–100 mg/m² IM bolus
- Or Infusion 55–100 mg/m²/day once stable
- Hydrocortisone 75–100 mg/m² IM bolus
Dose Calculation (Body Surface Area)
- BSA formula: √(Height (cm) × Weight (kg) ÷ 3600)
- BSA calculator or quick Table rapid estimates can be used in emergencies
Age-Based Initial Hydrocortisone Bolus (Succinate)
| Age Group | Initial Bolus | Infusion Rate |
| < 6 months (infants) | 12.5 mg | 1 mL/hr |
| Pre-schoolers (~2 years) | 25 mg | 2 mL/hr |
| Older children (~5 years) | 50 mg | 3 mL/hr |
| 10 years+ | 100 mg | 5 mL/hr |
Special Considerations
- Presumed adrenal insufficient patient (e.g., after CNS tumour resection) may also need coverage
- If raised ICP, consider Dexamethasone (high potency compared to hydrocortisone, but no mineralocorticoid effect)
- Always review steroid plan in light of ACTH deficiency, especially after surgery, as it may manifest weeks to months later
From my own clinical encounters, I’ve seen that early use of hydrocortisone succinate and aggressive fluid resuscitation often prevents rapid deterioration. One missed bolus or underestimation of dose can make recovery far harder.
B – Moderately Unwell
A stable patient who is still unwell, often with fever and reduced activity, but able to tolerate oral hydrocortisone, can usually be managed without aggressive IV intervention.
Steroid Dosing
- Give oral hydrocortisone 50 mg/m²/day
- This is typically 5x the normal total daily dose
- Divide into 4–5 doses across the day:
- Breakfast
- Lunch
- Afternoon tea
- Dinner
- Bedtime
- Breakfast
Supportive Care
- For Gastroenteritis with mild diarrhoea, encourage oral fluids
- If unable to maintain hydration, start IV or IM hydrocortisone as outlined above
In my own experience, parents often find the five times dosing tricky, but spacing it evenly through meals and bedtime helps adherence. Careful monitoring ensures the patient stays stable and avoids progressing to crisis.
C – Mildly Unwell
When a child has a respiratory or ear infection, with fever, occasional vomiting or diarrhoea, but still looks well, the approach is less aggressive.
Management
- Continue normal maintenance doses of steroid without increasing
- Treat infection with appropriate antibiotics if indicated
- Monitor for changes—if illness degrees in severity, escalate to moderate or severe protocol
In practice, most children in this group recover smoothly as long as the maintenance doses are not missed. The key is vigilance—what looks well today can shift quickly with fever or GI symptoms.
D – Elective Surgical Procedures
In simple elective surgery, patients with adrenal insufficiency need increased oral hydrocortisone for 24–48 hours, usually 2–3x the normal dose, depending on the onset and type of procedure. For very minor interventions like gastroscopy, where the Nil by mouth (NBM) period is short, this increase often suffices. Always discuss with the anaesthetist before the procedure, since even “minor” operations can turn into an acute prolonged illness situation.
Peri-operative Stress Steroids
| Stage | Route & Regimen | Notes |
| PRE-operatively | Single bolus of hydrocortisone (dose based on weight (kg) or age (yrs)) | If PO tolerated, give oral; if NBM, give IV |
| INTRA-operatively | Rate infusion in 50 mL saline, mg/hr as per body weight | Maintain coverage during anaesthesia |
| POST-operatively | Maintenance IV fluid with NaCl + glucose | Continue until patient is stable, then switch back to oral |
Practical Notes
- If unknown dosing, estimate by age or use 10 mg/m²/day as a safe fallback
- After recovery, switch back to normal oral dosing once eating resumes
- En route from recovery to the ward, make sure the infusion is continued
- For children, always tailor by weight (kg), and confirm with Table equivalents for accuracy
From my own experience, overlooking the peri-operative stress cover is one of the most common causes of adrenal crises post-surgery. A clear plan with the surgical and anaesthetic teams prevents last-minute confusion.
Examples
Case 1 – 12-year-old male with CAH
A 12-year-old male with Congenital Adrenal Hyperplasia (CAH) on steroids (fludrocortisone + hydrocortisone) presents with acute vomiting, abdominal pain, temperature 38.5°C, and is hypotensive.
- Administer 100 mg IM/IV hydrocortisone immediately
- Start continuous infusion 100 mg/m²/day
- Provide fluids and monitor closely until clinically stable
- Return to normally needed doses once crisis resolves
Case 2 – 9-month-old with congenital hypopituitarism
A 9-month-old infant with congenital hypopituitarism presents with upper respiratory infection and fever 38.3°C. He is on his usual medication: 2 mg AM, 1.25 mg midday, 1.25 mg night (total 5 mg/day hydrocortisone in 3 times doses).
- Continue maintenance dose while monitoring
- Seen by GP to investigate cause and ensure no progression to adrenal crisis
- Consider risk of multiple hormone deficiencies including AVP
- In settings like Starship ED, supportive care and close follow-up are critical until illness resolves
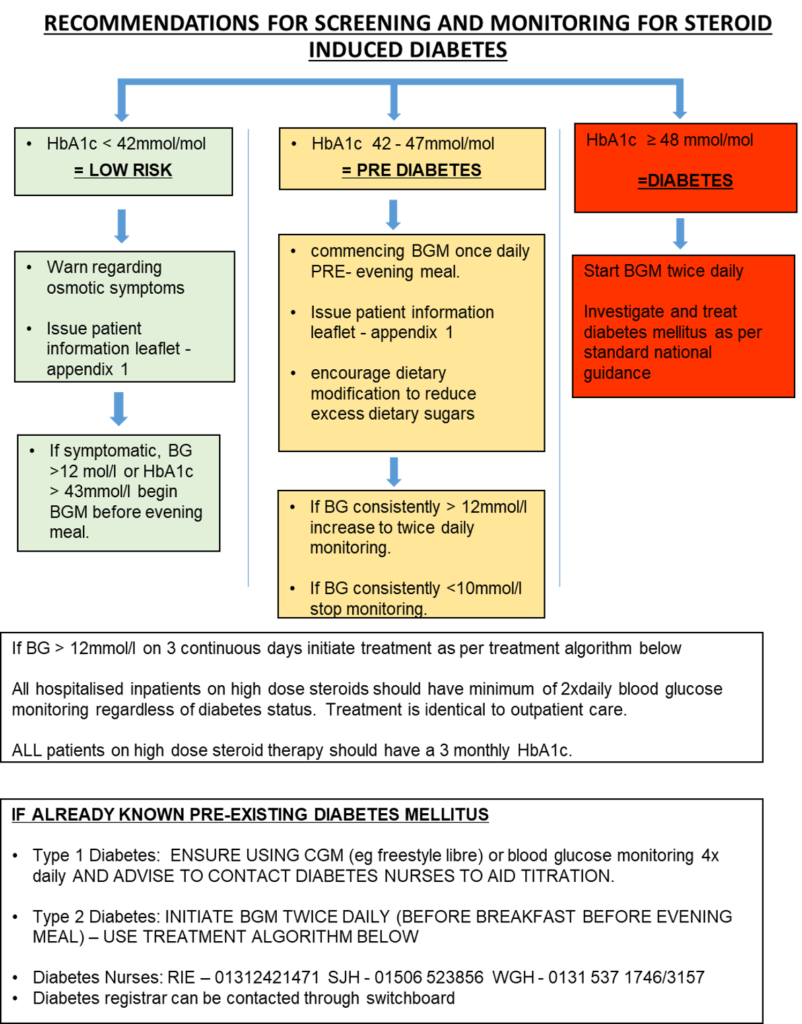
Steroid Potency
Different steroid preparations vary in their potency, glucocorticoid effect, and sodium retention. Understanding their equivalent doses in relation to hydrocortisone (cortisol) is essential for correct stress dose adjustments.
Steroid Potency Table
| Steroid | Potency (Glucocorticoid effect, relation to Hydrocortisone = 1.0) | Equivalent PO Dose (mg) | Equivalent Stress Dose (mg) | Sodium Retention |
| Cortisol / Hydrocortisone | 1.0 | 20 | 100 | Moderate |
| Cortisone | 0.8 | 25 | 125 | Moderate |
| Prednisone | 4 | 5 | 50 | Low |
| Prednisolone | 4–5 | 5 | 20 | Low |
| Methylprednisolone (Solumedrol) | 5 | 4 | 15 | 0 |
| Dexamethasone | 25–30 (≈80x) | 0.75 | 120 | None |
| 9α-Fluorocortisone (Florinef) | Mineralocorticoid only | N/A | N/A | Very High |
Key Notes
- Hydrocortisone (Cortisol) remains the reference standard for stress cover.
- Prednisone/Prednisolone: commonly used for maintenance but not ideal for emergencies.
- Methylprednisolone (Solumedrol): strong glucocorticoid, no mineralocorticoid activity.
- Dexamethasone: very high potency, no sodium retention, useful in specific cases (e.g., raised ICP).
- Florinef (Fludrocortisone): purely mineralocorticoid effect, used for long-term adrenal replacement alongside hydrocortisone.
From my clinical learning, keeping a ready reference table like this helps avoid under- or overdosing, especially when switching between individual preparations during emergencies.
Synacthen tests
Indication for Synacthen Test
The Synacthen test is used when there are clinical signs and symptoms suggestive of cortisol deficiency. It helps confirm:
- Primary hypoadrenalism
- Secondary hypopituitarism
- Suppression due to suppressive doses of glucocorticoids
Side Effects
A child may experience a brief warm sensation retrosternally during administration of Synacthen. This discomfort lasts about 2 minutes and usually resolves without intervention.
Preparation
- Ensure the child is off interfering steroids (unless testing replacement).
- Always inform referring doctor before starting.
- Fasting state not always required, but best if ambulant.
- Other stimulation tests (e.g., Growth Hormone) can be coordinated.
- Calculate surface area (BSA, m²):
BSA (m²) = √( Height(cm) × Weight(kg) / 3600 )
Equipment
- IV equipment with NaCl flushing set
- Blood tubes for samples (pre-labelled with times)
- Ampoule of Synacthen (tetracosactrin): synthetic ACTH 250 micrograms
- Accurate dose drawn based on child’s surface area (standard 1.73m²)
- Dilution method:
- Divide required 250 mcg into mL doses
- For Low dose test: add to 500 mL bag, mix, stable in refrigerator for 8 hours
- Prepare 1 mcg (2.2 mL) dose if needed
- Divide required 250 mcg into mL doses
Procedure
- Calculate dose of Synacthen based on BSA.
- Draw appropriately diluted solution.
- Insert IV line and withdraw zero (baseline) blood sample; label tube with exact time and cortisol measurement.
- For neonate where difficult to bleed, a random level may be considered.
- For neonate where difficult to bleed, a random level may be considered.
- Give tetracosactrin IV over a few seconds; ensure none is lost.
- Keep vein open with NaCl flush.
- Collect samples at timed intervals (e.g., 30 and 60 minutes draws).
- If IV access not possible, may administer IM.
- Remove IV line once finished.
- Additional access:
- For micro-collect testing (e.g., CAH), measure 17-hydroxyprogesterone at the same time point.
- For micro-collect testing (e.g., CAH), measure 17-hydroxyprogesterone at the same time point.
Emergency corticosteroid suplementation in patients taking exogenous corticosteroids
| Category | Initial | Subsequent |
| Minor procedure or surgery under local anesthesia (eg, inguinal hernia repair) | No extra supplementation is necessary | Continue normal dosing |
| Moderate surgical stress (eg, lower extremity revascularization, total joint replacement) | 50 mg hydrocortisone IV | 25 mg of hydrocortisone every eight hours for 24 hours. Resume usual dose thereafter. |
| Major surgical stress (eg, esophagogastrectomy, total proctocolectomy, open heart surgery) | 100 mg hydrocortisone IV | 50 mg every eight hours for 24 hours. Taper dose by half per day to maintenance level. |
Pediatric Dose
“Emergent Intramuscular Dosing can be given if child is not tolerating oral medications” [1]or unable to get IV within 15 minutes. IM hydrocortisone sodium succinate (Solu-Cortef)
- 25 mg for child 3 years and younger
- 50 mg for children >3 yrs – 12 years
- 100 mg for children 12 years and older.
👉 For the latest updates on finance, markets, and investment insights, check out https://fintechzoominsights.blog
FAQs About Stress Dose Steroids
Q1. What are stress dose steroids?
Stress dose steroids are extra doses of corticosteroids given during illness, surgery, or physical stress to patients with adrenal insufficiency.
Q2. When are stress dose steroids needed?
They are needed during fever, surgery, trauma, or severe illness to prevent adrenal crisis.
Q3. What is the dosage for stress dose steroids?
Dosage depends on the condition, age, and severity. Doctors usually adjust hydrocortisone or prednisone levels during stress.
Q4. Are stress dose steroids safe?
Yes, when prescribed correctly. However, long-term or incorrect use may lead to side effects like weight gain, mood changes, or high blood pressure.
Q5. Can stress dose steroids prevent adrenal crisis?
Yes, timely use of stress dose steroids is critical to preventing adrenal crisis in patients with Addison’s disease or adrenal insufficiency.